Losing yourself after neonatal intensive care – Sophie’s story
It’s hard bringing a premature baby home from hospital. The journey and worries go on. I’m trying to be honest with myself, I am struggling. Last December my son Bertie was born prematurely at just 27 weeks gestation. I’d had a complex pregnancy with bleeding from 13 weeks and placenta problems. I’d had numerous hospital stays and each time came away with different reasons. To this day the reason why is still unknown, but essentially my placenta was riddled with infections and I contracted sepsis.
Bertie was born by emergency C section at Gloucester Royal Hospital at 17.18. Later that evening, he was transferred to Bristol St Michaels, and then back to GRH after 8 days. I’ve said it a million times, and I’ll say it a million more, the doctors and nurses who work at both these hospitals are wonderful, wonderful humans who ultimately saved Bertie’s life. We are forever grateful.
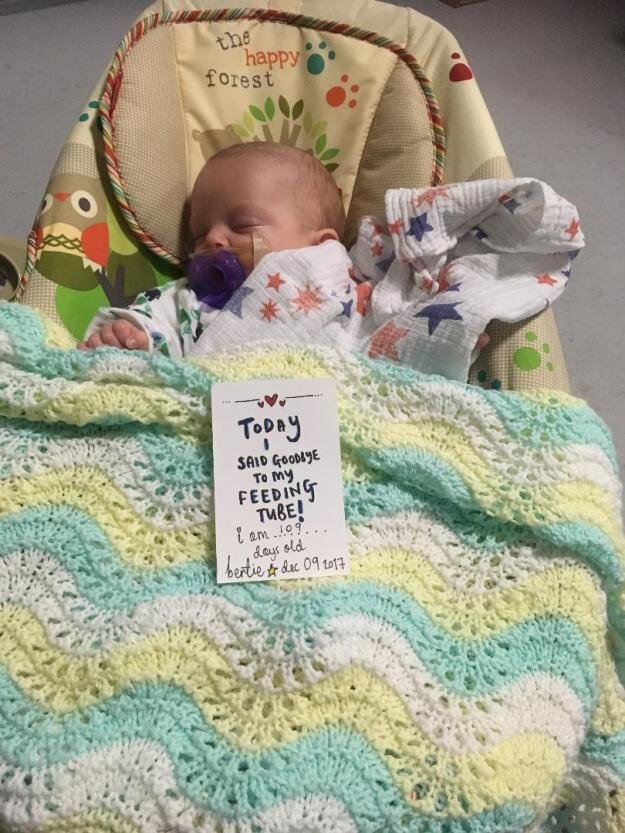
Bertie spent a total of 120 days in hospital. It really was one step forward, two (or what felt like many more) steps back. This is something we were told right from the beginning and it really is true. He had countless procedures, blood tests, x rays, ultra sounds and blood transfusions. He contracted the dreaded cold in hospital, twice. Intubated, CPAP, high flow and low flow; all terms I knew nothing about before, but will now forever be etched in my mind. NICU nurses become your most trusted friends and make such an impact on your day, time spent on the unit and, this sounds corny, but the rest of your life! I will never forget them. Other mums are like angels. Speaking to mums who “get it” is the most comforting thing. All NICU journeys are different but there seems to be an unspoken understanding of what goes on behind those closed doors. I have made friends for life and I am eternally grateful for their support. I hope I helped them, the way they help me.
We bought Bertie home on 8 April 2018. At last we could be together as a family of 4. Mike, Charlie, Bertie and me. I thought the stay in hospital was the hardest thing I’d ever done, juggling a toddler at home and a baby in hospital was heart breaking and watching your baby constantly fight is indescribable. Mike and I were like ships in the night. I’d be at the hospital during the day, he would go to work, then he’d go the hospital in the evening and I’d be home with Charlie. We’d be lucky to eat a microwave meal together! The uncertainty of Bertie’s health and development was always on my mind, but bringing home a premature baby who has chronic lung disease and required 24/7 oxygen, who is so susceptible to illnesses and who is “failing to thrive” was and is, much harder.
I cannot comprehend why being at home as a family would be harder than our time in hospital, but it is. I feel a huge amount of guilt for saying that, along with a lot of other things. Like not spending enough time with Charlie, not spending enough time with Bertie, not being a “good” wife, the list goes on. One of my biggest guilt is why couldn’t I carry Bertie to full term. I do know that it is not my fault and that I did nothing “wrong”, but I still feel guilt. I was told by a wonderful woman recently that we must accept our feelings and it is just how we feel. I am working on that.
We’ve been home for 7 months now. In that time we’ve had 2 overnight stays in hospital, endless appointments with physios, occupational therapists, dieticians and Bertie’s fantastic consultant. Home visits from our amazing respiratory nurse, which always felt like a visit from a friend, but also difficult visits from health visitors who had little understanding of pre term babies. I feel immense pressure for Bertie to be “well”. I worry. I am swamped by worry. Worry that he is not developing as he is should be, worry that he will have long term effects of being premature, worry that I’m not giving him enough attention, worrying about his weight, worry that he might get ill again, worrying about more hospital admissions and worry that in all this I’m neglecting his older brother Charlie. Going into the winter is an exceptionally worrying time, a simple cold could put Bertie in hospital. It’s already happened twice and it’s not even been the cough and cold season yet.
In August, amazingly Bertie was able to wean off his oxygen in the day. Then in October he has come off oxygen at night too. This was a massive milestone for Bertie! I was so pleased but with this came more anxiety. The oxygen is almost a safety net, a comfort maybe. Take it away, it’s another worry. A huge ongoing battle for Bertie is his weight and feeding, he takes very little milk and has very little food. He has awful reflux which is not helped by a persistent cough. Recently we had a particularly bad spell and he lost weight. I feel like we go round in circles and it is never ending.
There is a massive lack of understanding and knowledge about premature birth, our babies and life after NICU. By sharing our story I want to help people going through the same and give knowledge to others. One of my biggest frustrations is that I feel a lot of people assume that just because we are home now that Bertie is “fine” and like a “normal” baby. I hope this at least goes a little way in showing this is not the case.
Along with guilt and worry, I am filled with jealousy. When I walk through the supermarket and see a heavily pregnant woman, I feel jealous that they’ve carried their baby further than I did, jealous that they will have a new born baby to enjoy and jealous that they don’t know about the NICU experience. I then I feel bad for having those thoughts and feelings. Another seemingly never ending circle that I hope with time will end.
I am grateful beyond belief to the wonderful NHS. It is still early days for me. I have two beautiful sons, I am so lucky, but also feel like I have lost who I am. In sharing our story hope to find myself again.
With thanks to Sophie for sharing her story, raising awareness of the ongoing needs of families following premature birth and neonatal intensive care.